Freezing eggs in Illinois can cost between $10,000 and $15,000 per cycle, with medications adding $3,000 to $6,000 and annual storage fees of $1,000+. However, Illinois offers a fertility insurance mandate under Public Act 102-0170, requiring many employer-sponsored plans to cover medically necessary fertility preservation for treatments like chemotherapy that risk infertility.
Key points:
- Insurance Coverage: Applies to employer-sponsored plans with over 25 employees, excluding self-funded plans, small businesses, and religious organizations.
- Medically Necessary vs. Elective: Coverage is only for medically necessary cases (e.g., cancer treatment). Elective egg freezing, for future family planning, is not covered.
- Out-of-Pocket Costs: Even with coverage, medications and storage fees are often excluded.
To understand your costs:
- Review your insurance policy for fertility benefits.
- Confirm with your insurer if your plan complies with Illinois’ mandate.
- Consult financial counselors at fertility clinics for cost breakdowns and insurance navigation.
Illinois residents benefit from this mandate, but exclusions and partial coverage mean out-of-pocket costs can still be significant.
Preserving Fertility During Cancer Treatment: Options, Costs & Success Rates | Cancer Straight Talk
Illinois Fertility Preservation Mandate
The fertility preservation mandate (215 ILCS 5/356z.32), which took effect on January 1, 2019, focuses on covering egg freezing for individuals undergoing medical treatments that could result in infertility. This mandate is separate from the broader infertility treatment mandate, which addresses conditions like IVF for those already diagnosed as infertile.
What the Mandate Covers
This law requires insurance policies to include coverage for "standard fertility preservation services" when a medical treatment has the potential to cause iatrogenic infertility – infertility resulting from medical interventions such as surgery, radiation, or chemotherapy. According to the statute:
An individual or group policy of accident and health insurance… must provide coverage for medically necessary expenses for standard fertility preservation services when a necessary medical treatment may directly or indirectly cause iatrogenic infertility to an enrollee.
The mandate overrides typical insurance exclusions for egg cryopreservation and storage if the treatment poses a risk to fertility. Coverage must align with evidence-based standards set by organizations like the American Society for Reproductive Medicine (ASRM) or the American Society of Clinical Oncology (ASCO). Insurers are prohibited from discriminating based on factors such as age, sex, sexual orientation, marital status, or life expectancy when determining coverage. The key requirement for coverage is the medical necessity of the treatment.
Who Qualifies for Coverage
You may qualify for mandated coverage if your medical treatment puts your fertility at risk. This often applies to cancer patients undergoing chemotherapy or radiation, individuals receiving treatments harmful to reproductive health, or those undergoing other gonadotoxic therapies. Typically, coverage is granted for life-threatening diagnoses like cancer.
To be eligible, your insurance plan must be fully insured and issued in Illinois. The mandate applies to individual and group policies amended, delivered, issued, or renewed after January 1, 2019. For broader infertility treatment coverage, such as IVF, your employer must have more than 25 employees. Starting January 1, 2026, expanded mandates will apply to all group health insurance policies in Illinois that offer pregnancy benefits.
What the Mandate Doesn’t Cover
Although the mandate ensures coverage for medically necessary preservation services, it does not extend to elective procedures. Elective egg freezing, often referred to as "social egg freezing", for reasons like career planning or delaying parenthood, is not included. The law strictly applies to fertility preservation procedures deemed medically necessary due to treatments that threaten fertility.
Certain plans are exempt from the mandate. Self-insured (self-funded) plans, which are governed by federal ERISA law, do not fall under state requirements. These plans are common among large corporations that pay claims directly instead of using an insurance carrier. Similarly, religious organizations may opt out if the coverage conflicts with their teachings. While Illinois Medicaid may cover some fertility preservation services when medically necessary, it does not include elective egg freezing.
Other exclusions are sterilization reversal, non-medical costs for donors or surrogates, travel expenses within 100 miles of your home, and experimental treatments.
Egg Freezing Costs Without Full Coverage
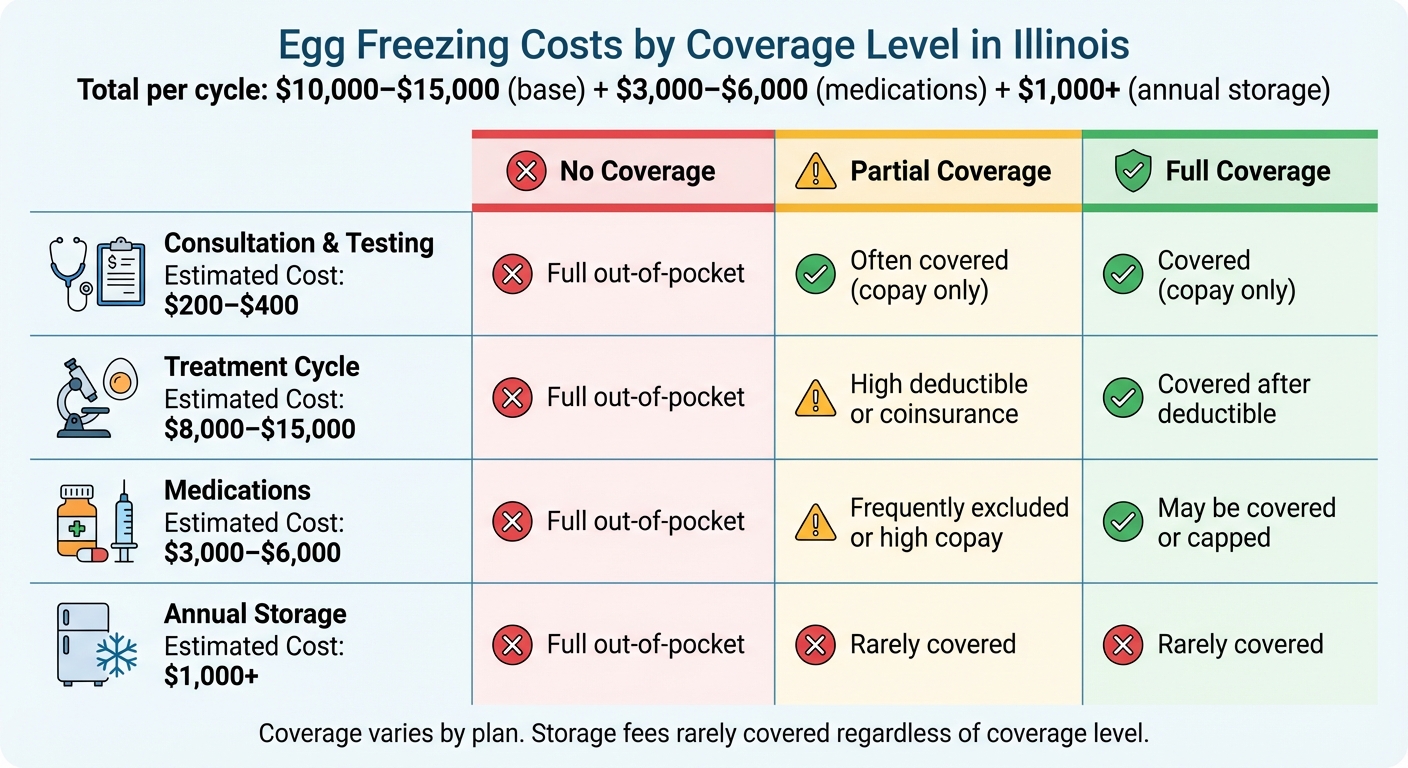
Egg Freezing Costs in Illinois by Insurance Coverage Level
Even with mandates in place, the out-of-pocket expenses for egg freezing can be steep, especially when insurance coverage is limited or unavailable. This is particularly true for elective procedures or plans that fall outside state requirements. Breaking down the costs can help you better prepare financially. Here’s a closer look at the typical expenses for egg freezing in Illinois.
Cost Breakdown by Service
Lauren Makler, CEO of Cofertility, points out that medications alone can add between $3,000 and $6,000 to the base cost of a cycle.
Here’s what you can expect to pay for various components:
- Initial consultation and fertility testing: Between $200 and $400.
- Base cycle fee: This includes monitoring, egg retrieval, vitrification, and anesthesia, with costs ranging from $8,000 to $15,000. For example, the Advanced Fertility Center of Chicago starts at $8,000 and includes one year of storage, while CNY Fertility offers packages starting at $2,999 [3, 18, 19].
- Ovarian stimulation medications: Costs range from $3,000 to $6,000 per cycle [3, 18].
- Annual storage fees: Typically over $1,000 in the Chicago area [3, 19].
- Future costs: Processes like thawing, fertilization, and embryo transfer can add $2,500 or more.
Covered vs. Uncovered Costs
The financial burden becomes clearer when examining the difference between full, partial, and no insurance coverage. Partial coverage can sometimes be misleading. Fertility Centers of Illinois explains:
Some plans are ‘diagnostic only’ which means that they only cover testing that is done before starting fertility treatment. Your plan may or may not cover aspects of treatment such as medications, outside monitoring, cryopreservation of embryos or genetic testing.
In practical terms, this could mean that while your initial consultation and testing are covered, you might still face full costs for the actual treatment cycle, medications, and storage. The table below highlights how costs vary based on your level of insurance coverage:
| Expense Category | Estimated Cost | No Coverage | Partial Coverage | Full Coverage |
|---|---|---|---|---|
| Consultation & Testing | $200–$400 | Full out-of-pocket | Often covered (copay only) | Covered (copay only) |
| Treatment Cycle | $8,000–$15,000 | Full out-of-pocket | High deductible or coinsurance | Covered after deductible |
| Medications | $3,000–$6,000 | Full out-of-pocket | Frequently excluded or high copay | May be covered or capped |
| Annual Storage | $1,000+ | Full out-of-pocket | Rarely covered | Rarely covered |
For those with partial coverage, the highest out-of-pocket expenses often come from medications and storage fees, as these are rarely reimbursed [3, 8]. Even if the retrieval procedure itself is covered, pharmacy benefits for specialty medications may still be billed separately [3, 8].
sbb-itb-a729c26
Insurance Providers and Plans That Cover Egg Freezing in Illinois
Providers Offering Coverage
In Illinois, major insurance companies like Aetna, Blue Cross Blue Shield of Illinois, UnitedHealthcare, Cigna, and Humana provide coverage for egg freezing when it’s deemed medically necessary under state mandate conditions. These plans, which may come as HMOs, POS, or PPO options, typically include fertility preservation benefits for situations where medical treatments – such as chemotherapy – might result in iatrogenic infertility. Additionally, some smaller regional insurers may also meet these requirements.
Coverage usually falls into two categories: medically necessary preservation and infertility diagnosis treatment, each with distinct eligibility requirements.
Some insurers, like Aetna, may require members to complete certain pre-tests or participate in fertility programs before starting treatment. On top of that, some employers offer supplemental fertility benefits through providers like Progyny, Maven, or WINFertility. However, the specifics of these benefits vary depending on the employer.
Given the range of options and requirements, having expert guidance can make navigating these plans much simpler.
How Illinois Health Agents Can Help

Illinois Health Agents play a key role in simplifying the process of finding the right coverage. They assist individuals and employers in identifying ACA-compliant plans and group health options that align with Illinois’ state mandates. Their expertise helps determine whether an employer’s health plan is fully insured (and subject to state laws) or self-insured (which may not follow state mandates). This distinction is crucial as it directly affects eligibility for fertility benefits.
For businesses with over 25 employees, Illinois Health Agents work with employers to select group health plans that include the mandated fertility preservation benefits. They also ensure the plan complies with state requirements by verifying network coverage, confirming any necessary pre-testing, and carefully reviewing the Certificate of Coverage to confirm it includes provisions for fertility preservation and iatrogenic infertility.
How to Determine Your Egg Freezing Costs and Coverage
Review Your Insurance Policy
Start by checking with your HR department to see if your employer (with more than 25 employees) offers a fully insured plan that complies with the Illinois mandate. Keep in mind that self-insured plans are not bound by state mandates, so they might not cover egg freezing, even if you work for a large company.
Next, get a copy of your Summary of Benefits and search for terms like fertility preservation, cryopreservation, or iatrogenic infertility. Some plans may only cover diagnostic testing but exclude the actual egg freezing procedure. Pay close attention to the details – look for any age restrictions, waiting periods, or lifetime maximum benefits. Many Illinois plans cap fertility benefits between $10,000 and $25,000.
Once you’ve reviewed your policy, reach out to your insurer to clarify the specifics.
Contact Your Insurance Provider
Use the phone number on your insurance card to contact your provider and confirm whether your plan complies with Public Act 102-0170. This law, which went into effect in Illinois in 2022, expanded fertility coverage. To get clear answers, Howard Brown Health suggests asking:
"I am interested in learning more about coverage for infertility treatments in my insurance plan. Specifically, a new law, Public Act 102-0170, went into effect in Illinois on January 1, 2022… Is my plan in compliance with this new law?"
Be sure to ask about any pre-authorization requirements, specialty pharmacy rules, deductibles, or copays. Request written confirmation of all the details for your records.
Work with Fertility Clinic Financial Counselors
Financial counselors at fertility clinics can help you navigate coverage gaps and provide accurate cost estimates. According to Fertility Centers of Illinois:
"Most patients have some coverage for infertility treatment. Our financial counselors will work closely with you to ensure that you are making the most of your insurance coverage."
These counselors can also verify whether the clinic is in-network with your insurance plan, which can make a big difference in your out-of-pocket expenses. Some insurance plans only cover in-office procedures and ultrasounds, while excluding IVF lab and surgery center fees. Understanding these nuances upfront can help you plan your budget more effectively.
Get Help from Illinois Health Agents
If you’re self-employed or work for a small business, Illinois Health Agents can assist you in finding state-compliant health plans. They can compare options during open enrollment to identify plans with better fertility benefits. Additionally, they can verify whether your employer’s plan is exempt from the Illinois mandate and help employers choose group health plans that include fertility preservation coverage.
Conclusion
In Illinois, egg freezing becomes significantly more affordable when insurance coverage is involved, compared to paying entirely out-of-pocket. Thanks to Public Act 102-0170, employer group health plans covering businesses with more than 25 employees are now required to include fertility preservation services, such as egg freezing, under specific conditions. This opens the door for many Illinois residents to access coverage for up to four egg retrievals, with the option for two additional retrievals if a live birth is achieved. These advancements reflect the broader details on mandates, costs, and coverage options previously discussed.
That said, not all plans qualify under this mandate. Even those that do may still leave you with out-of-pocket costs for items like lab fees, anesthesia, or medications. Additionally, some plans impose lifetime maximum benefits ranging from $10,000 to $25,000, which could limit coverage.
To avoid unexpected financial hurdles, take these steps: First, confirm whether your employer’s plan complies with the Illinois mandate and review your policy for exclusions or limitations. Reach out to your insurance provider to clarify pre-authorization requirements, deductibles, and copays. Fertility clinic financial counselors can also help pinpoint any gaps in coverage. For those who are self-employed, work for small businesses, or need extra support, Illinois Health Agents can assist in finding state-compliant plans with better fertility benefits. They can also help verify whether your employer’s plan is exempt from the mandate and guide you through comparing options during open enrollment. Taking these steps can help ensure you’re well-prepared to make informed decisions about egg freezing without facing unexpected costs.
FAQs
What does ‘medically necessary’ mean for egg freezing coverage in Illinois?
In Illinois, the term "medically necessary" for egg freezing applies when the procedure is required to safeguard fertility before undergoing medical treatments that might cause infertility. This often includes treatments like chemotherapy, radiation, or surgeries that could potentially damage the reproductive system.
State laws mandate that insurers cover the costs of egg freezing and related procedures in these situations. This coverage aligns with evidence-based care standards set by respected organizations such as the American Society for Reproductive Medicine (ASRM) and the American Society of Clinical Oncology (ASCO). If the procedure is determined to be medically necessary, insurers are prohibited from denying coverage.
Do any insurance plans in Illinois cover elective egg freezing?
Yes, some insurance plans in Illinois might include coverage for elective egg freezing, but it largely depends on your specific provider and plan. Illinois law mandates insurance to cover medically necessary fertility preservation, but certain employer-sponsored plans – like those offered by Aetna, Blue Cross Blue Shield, or UnitedHealthcare – often extend benefits to elective egg freezing as well.
To confirm if your plan includes this coverage, take a closer look at your insurance policy or reach out to your provider directly. It’s also worth checking with your employer to see if fertility benefits are part of your plan. Keep in mind that even with coverage, you might still face out-of-pocket expenses, depending on factors like your deductible and copay requirements.
How can I check if my employer’s insurance plan covers fertility preservation under Illinois law?
To figure out if your employer’s health plan complies with Illinois’s fertility preservation mandate, start by checking the plan documents. You can request the Summary of Benefits & Coverage (SBC) or the full policy details from your HR department or benefits portal. Specifically, look for any mention of coverage for fertility preservation services, such as egg or embryo freezing, particularly if a medical treatment might lead to iatrogenic infertility (infertility caused by medical procedures like chemotherapy or surgery).
Under Illinois law, group health plans covering more than 25 employees are required to provide these services if the plan was issued, renewed, or amended on or after January 1, 2019. If you’re uncertain, reach out to your insurer’s member services or your benefits administrator to confirm whether your plan adheres to Illinois’s fertility preservation rules. You can also ask your HR team for more details or, if necessary, file a formal inquiry with the Illinois Department of Insurance.


Recent Comments